
Rare thoracic findings of catamenial pneumothorax due to repeated relapse and spontaneous remission: a case report
Highlight box
Key findings
• The repeated pneumothorax and spontaneous remission of catamenial pneumothorax created a rare intrathoracic finding that required surgical repair.
What is known and what is new?
• Repeated slight pneumothorax is a characteristic of catamenial pneumothorax.
• Repeated episodes of minor pneumothorax and the process of spontaneous remission formed multiple adhesions in the thoracic cavity. Lung dilation was incomplete and thoracic cavity was divided into many regions that finally needed surgical treatment.
What is the implication, and what should change now?
• Patients of catamenial pneumothorax should be observed regularly over a long period of time until menopause.
Introduction
Catamenial pneumothorax is a relatively rare disease that was first reported by Maurer et al. in 1958 (1). It is characterized by pneumothorax that occurs in accordance with the menstrual cycle (2,3). However, the mechanism of occurrence has not been fully revealed. Possible mechanisms are: (I) Endometrial cells adhere to the diaphragm, resulting in a hole in the diaphragm during menstruation. It occurs when air flows into the abdominal cavity from the fallopian tube through the defect hole and flows into the thoracic cavity. (II) Endometrial cells adhere to the visceral pleura through blood circulation and the pleura ruptures during the menstrual period. (III) Rupture occurs in the alveoli as a result of constriction of blood vessels and airways due to the production of prostaglandins, which increase during the menstrual period. Repeated slight pneumothorax without subjective symptoms is a characteristic of catamenial pneumothorax. After the diagnosis of catamenial pneumothorax, appropriate treatment including hormone treatment is required to stop repeated pneumothorax. Rare intrathoracic finding, an extensive adhesion of lung, has never been reported as a clinical finding of catamenial pneumothorax before. In this report, we discuss the course of catamenial pneumothorax that has been left untreated for several years without hormone treatment. We present this case in accordance with the CARE reporting checklist (available at https://ccts.amegroups.com/article/view/10.21037/ccts-23-7/rc).
Case presentation
A 44-year-old woman was admitted to the hospital, in November 2020, with a complaint of right-sided chest pain on the third day of menstruation. Chest X-ray showed mild collapse of the right lung (Figure 1A). However, chest computed tomography (CT) revealed that the right lung adhered irregularly to the chest wall at several sites, and lung dilation was incomplete. The right lung was widely adhered in multiple locations due to membranous tissue that spread from the lung apex to the lung base. The lungs were unable to fully expand or collapse completely. The thoracic cavity was divided into many regions; however, no emphysematous cysts were identified (Figure 1B).
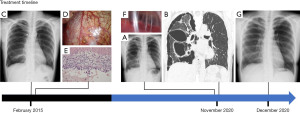
Furthermore, 5 years before this event, in February 2015, at the age of 39, she was diagnosed with right pneumothorax (Figure 1C). She underwent surgery for right pneumothorax, and several brown nodes suspected to be endometrial tissues were observed on the diaphragm (Figure 1D). Partial diaphragmatic resection was performed, pathological examination revealed endometrial tissue, and catamenial pneumothorax was diagnosed (Figure 1E). Furthermore, a dark brown change on the visceral pleura was observed macroscopically, and partial lung resection was performed; however, there were no significant histological findings. No adhesions were observed in the thoracic cavity during surgery. No pleural symphysis treatment was performed during the first thoracoscopy. Hormone therapy was not desired after the pneumothorax was relieved, and regular outpatient visit was completed in 1 year. Hormone treatment was planned in case of recurrence of pneumothorax. During the 1-year period, with a regular visit to the hospital and chest X-rays every month, there were no noteworthy findings in either subjective or image findings. She had no history of smoking, and no significant abnormalities were identified on laboratory tests and physical examination. She had no past incidents of pneumothorax, or any chest discomfort related to her menstrual cycle.
This time, as she was admitted to our hospital, we suspected she had a recurrence of catamenial pneumothorax. Chest tube drainage was necessary, but it was difficult to perform the same at the patient’s bedside. Therefore, adhesion detachment and drainage were performed during thoracoscopic surgery. Thoracoscopic surgery was performed to determine disease etiology and to perform effective drainage to allow for complete lung dilation. Membrane-like adhesions were widespread from the lung apex to the lung base (Figure 1F). No air leaks were found during the operation, and no nodules or pits suspected to be endometrial tissue were found on the diaphragm. A dark brown change was observed on the visceral pleura, but histological examination did not reveal endometrial tissue. Furthermore, no lung cysts were identified. A valid drain was placed, and the operation was completed with no adverse event. A few days after surgery, X-ray image of the lung showed complete lung re-expansion and the patient’s symptoms relief (Figure 1G). Additional treatment for hormone therapy was again not desired and was not administered. There was no recurrence of pneumothorax 1 year after the surgery. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent for publication of this case report and accompanying images was not obtained from the patient or the relatives after all possible attempts were made.
Discussion
Catamenial pneumothorax is a rare primary pneumothorax that mostly occurs in a productive age female. Catamenial pneumothorax is characterized by pneumothorax that occurs in accordance with the menstrual cycle due to collapse of the endometrium in the thoracic cavity. Catamenial pneumothorax occurs within a few days before and after menstrual onset and occurs most of the time on the right side (4-6). Lung collapse and subjective symptoms associated with catamenial pneumothorax are mild and are characterized by repeated spontaneous relief and recurrence of slight pneumothorax (7-9).
Diagnostic methods for catamenial pneumothorax include medical history, image findings and direct view of blueberry spots and histopathological findings of endometrial lesion through thoracoscopic surgery. Endometrial cells adhered to the visceral pleural or the diaphragm in some way rupture during the menstrual period and caused pneumothorax (2,3).
There is still no consensus about the treatment. Treatment methods for catamenial pneumothorax include thoracoscopic surgery and hormone therapy. Thoracoscopic surgery involves cutting and suturing the defect in the diaphragm and sometimes using talc pleurodesis (10). Hormone therapy is performed with a gonadotropin releasing hormone agonist (11).
Owing to the frequent recurrence of mild pneumothorax, it is difficult to achieve complete healing with surgical treatment alone. Surgery is performed only diagnostically (12).
Hormonal therapy, though it cannot make a complete regression, controls endometrial tissues in the thoracic cavity and decreases pneumothorax recurrence. Although hormone therapy has side effects, hormone therapy should be added after surgical diagnosis to prevent recurrence (9). Recurrence is often observed in patients who did not receive hormone therapy due to their refusal or the side effects of the treatment (13).
In the case of our patient, the rare thoracic endometrial lesions on the visceral pleura may have ruptured to cause slight asymptomatic pneumothorax and adhesion to the chest wall during spontaneous relief. Even in the event of a pneumothorax, the lung repeatedly adhered to the chest wall and was incompletely dilated.
At the time of the first surgery, histological examination confirmed endometrial tissue only on the diaphragm, but the lesion may have also been present on the visceral pleura. During the second operation, endometrial tissue could not be confirmed via histological examination as the operation was performed during the menstrual period (14-16). It was reported that endometrial tissue falls off and regresses during the intermittent period of menstruation and that endometrial tissue is often not found in the resected lesions (17).
The patient had undergone diaphragm and partial lung resections for catamenial pneumothorax 5 years before being admitted to our hospital, and hormone therapy was not performed. Regular consultation was terminated 1 year after the operation. The rare thoracic cavity findings in this patient may be due to repeated spontaneous remission after the recurrence of mild pneumothorax.
Limitation
This study is just a report on an individual case, and it is difficult give a certain interpretation based on this case alone. But through this case, it became clear once again that menstrual pneumothorax recurs repeatedly, and that long-term observation is necessary to treat recurrences appropriately.
Conclusions
It may be difficult for busy young women to continue regular hospital visits if there are no subjective symptoms, no abnormalities identified from examinations, and no intentions to receive hormone therapy. However, patients with thoracic endometriosis-related pneumothorax, catamenial pneumothorax should be observed regularly over a long period of time until menopause to avoid unnecessary surgical intervention.
Acknowledgments
The authors thank Enago (www.enago.jp) for the English language review.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://ccts.amegroups.com/article/view/10.21037/ccts-23-7/rc
Peer Review File: Available at https://ccts.amegroups.com/article/view/10.21037/ccts-23-7/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://ccts.amegroups.com/article/view/10.21037/ccts-23-7/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent for publication of this case report and accompanying images was not obtained from the patient or the relatives after all possible attempts were made.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Maurer ER, Schaal JA, Mendez FL Jr. Chronic recurring spontaneous pneumothorax due to endometriosis of the diaphragm. J Am Med Assoc 1958;168:2013-4. [Crossref] [PubMed]
- Gil Y, Tulandi T. Diagnosis and Treatment of Catamenial Pneumothorax: A Systematic Review. J Minim Invasive Gynecol 2020;27:48-53. [Crossref] [PubMed]
- Quercia R, De Palma A, De Blasi F, et al. Catamenial pneumothorax: Not only VATS diagnosis. Front Surg 2023;10:1156465. [Crossref] [PubMed]
- Bricelj K, Srpčič M, Ražem A, et al. Catamenial pneumothorax since introduction of video-assisted thoracoscopic surgery: A systematic review. Wien Klin Wochenschr 2017;129:717-26. [Crossref] [PubMed]
- Nezhat C, Lindheim SR, Backhus L, et al. Thoracic Endometriosis Syndrome: A Review of Diagnosis and Management. JSLS 2019;23:e2019.00029.
- Shikino K, Ohira Y, Ikusaka M. Catamenial Pneumothorax. J Gen Intern Med 2016;31:1260. [Crossref] [PubMed]
- Kronauer CM. Images in clinical medicine. Catamenial pneumothorax. N Engl J Med 2006;355:e9. [Crossref] [PubMed]
- Rousset P, Rousset-Jablonski C, Alifano M, et al. Thoracic endometriosis syndrome: CT and MRI features. Clin Radiol 2014;69:323-30. [Crossref] [PubMed]
- Visouli AN, Zarogoulidis K, Kougioumtzi I, et al. Catamenial pneumothorax. J Thorac Dis 2014;6:S448-60. [PubMed]
- Pratomo IP, Putra MA, Bangun LG, et al. Video-assisted surgical diagnosis and pleural adhesion management in catamenial pneumothorax: A case and literature review. Respirol Case Rep 2023;11:e01123. [Crossref] [PubMed]
- Hirsch M, Berg L, Gamaleldin I, et al. The management of women with thoracic endometriosis: a national survey of British gynaecological endoscopists. Facts Views Vis Obgyn 2021;12:291-8. [PubMed]
- Nair SS, Nayar J. Thoracic Endometriosis Syndrome: A Veritable Pandora's Box. J Clin Diagn Res 2016;10:QR04-8. [Crossref] [PubMed]
- Sharma N, Todhe P, Ochieng P, et al. Refractory thoracic endometriosis. BMJ Case Rep 2020;13:e235965. [Crossref] [PubMed]
- Haga T, Kataoka H, Ebana H, et al. Thoracic endometriosis-related pneumothorax distinguished from primary spontaneous pneumothorax in females. Lung 2014;192:583-7. [Crossref] [PubMed]
- Fukuoka M, Kurihara M, Haga T, et al. Clinical characteristics of catamenial and non-catamenial thoracic endometriosis-related pneumothorax. Respirology 2015;20:1272-6. [Crossref] [PubMed]
- Tsuboshima K, Matoba Y, Wakahara T, et al. Natural history of bulla neogenesis for primary spontaneous pneumothorax: a propensity score analysis. Gen Thorac Cardiovasc Surg 2019;67:464-9. [Crossref] [PubMed]
- Mecha E, Makunja R, Maoga JB, et al. The Importance of Stromal Endometriosis in Thoracic Endometriosis. Cells 2021;10:180. [Crossref] [PubMed]
Cite this article as: Osako T, Takuwa T. Rare thoracic findings of catamenial pneumothorax due to repeated relapse and spontaneous remission: a case report. Curr Chall Thorac Surg 2024;6:2.


