Spontaneous pneumomediastinum: a rare cause of dyspnea
Introduction
Acute thoracic pain and dyspnea can be caused by a wide variety of diseases. Pneumomediastinum is a rare cause of these symptoms and is often related with trauma, infections, medical procedures or surgery. Diagnosis of a spontaneous pneumomediastinum can only be made if any other possible cause has been excluded. Spontaneous pneumomediastinum (SPM) is benign condition which does not need any further treatment.
Case presentation
An 18-year-old male presented in the emergency department with a sore throat, dyspnea and thoracic pain since 1 day. He did not have any relevant medical history, no history of drug abuse, and no abnormal activity in the days before the admission.
Clinical investigation showed no fever, normal respiratory rate of 14/min without using accessory respiratory muscles and a normal heart rate and blood pressure. Chest auscultation revealed normal bilateral breathing sounds and normal cardiac auscultation without Hamman’s sign. Blood tests only showed a slightly elevated leukocytosis (11,600/µL) without any other deviations.
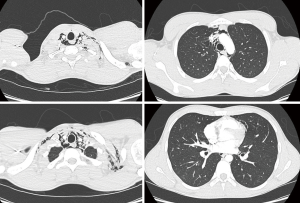
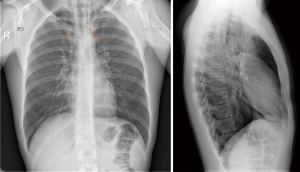
On chest X-ray (Figure 1), a “V sign of Naclerio” was seen, suggestive for the presence of a pneumomediastinum. Next, a thoracic CT scan was performed to rule out any serious cause of pneumomediastinum (Figure 2). This could not indicate any cause of pneumomediastinum, and a tentative diagnosis of SPM was withheld. The patient was admitted to the ward for observation with nil per os management, and prophylactic intravenous antibiotics were administered in case of a latent esophageal perforation that was missed on initial imaging.
The patient had an uneventful stay on the ward, with symptoms that remained unchanged during the next two days. Repeat chest X-ray was unchanged. Two days after admission, a chest-CT with peroral contrast was performed to investigate the presence of an esophageal perforation, which could not be found. The tentative diagnosis of SPM was therefore confirmed and the patient left the hospital in good general condition.
Discussion
Pneumomediastinum is defined as the presence of air in the mediastinum. This can occur spontaneously, without any clear precipitating events. Secondary pneumomediastinum can be caused by trauma, surgery, medical procedures or infection. If a pneumomediastinum is found, it is of utmost importance to rule out any serious cause, since a pneumomediastinum can be a sign of damage to the mediastinal structures, such as the esophagus or trachea. If these causes are excluded, the diagnosis of SPM can be made.
Pneumomediastinum was first described by René Laennec in 1819 and “spontaneous mediastinal emphysema” was reported by Louis Hamman in 1939 (1), stating that the term spontaneous was justified when “the pulmonary alveoli rupture in healthy individuals”. The pathophysiology was explained by Macklin (2), emphasizing the importance of a decrease in pressure gradient between the lung alveoli and the interstitial tissue which may lead to alveolar rupture. Leakage of air through the interstitium and bronchovascular sheath leads to the presence of air in the mediastinum. Situations in which this may occur, are a Valsalva maneuver, when intra-alveolar pressure increase, or Mueller maneuver in bronchial asthma (inspiratory effort with blocked airway), when pleural pressure drops (3). Some reports state that SPM occurs more frequently in males and in thin, young adults (3).
Presenting symptoms are thoracic pain (54–65%), dyspnea (39–51%), cough (32%) and neck pain (29%) (3-5). Clinical investigation may reveal crepitus secondary to subcutaneous emphysema, and a Hamman’s sign, which is crepitus heard with heart beat on cardiac auscultation. Diagnosis is made through imaging, either with chest X-ray showing a “V sign of Naclerio”, radiolucent streaks of air outlining the mediastinal structures often extending to the neck, or a thoracic CT scan, which remains the gold standard (3).
The presence of SPM has been reported in association with asthma, straining during exercise, diabetic ketoacidosis, childbirth, severe cough and vomiting, inhalation of drugs such as marihuana and cocaine, plying of wind instruments and sexual activity (3-5). Yet, in a large portion of patients (8–51%), no clear eliciting event can be found (3).
SPM is a benign condition with excellent prognosis and very low recurrence rates (5). Patients presenting with pneumomediastinum are often subjected to a large amount of technical investigations to rule out any serious cause of pneumomediastinum. They are often admitted with restricted oral intake and antibiotics. Recent studies have shown that these investigations are often negative and that most of the patients don’t need this extensive work-up. Two recent reports summarized risk factors for further investigation and proposed an algorithm for the management of pneumomediastinum (3,4). In anticipation, the patients are often admitted with restricted oral intake and antibiotics.
In case of SPM, if damage to important mediastinal structures such as trachea and esophagus are excluded, a short observation either in- or outpatient with supportive measures such as rest and pain control, is sufficient.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hamman L. Spontaneous mediastinal emphysema. Bull Johns Hopkins Hosp 1939;64:1-21.
- Macklin C. Transport of air along sheaths of pulmonic vessels from alveoli to mediastinum. Arc Intern Med 1939;64:913-26. [Crossref]
- Bakhos CT, Pupovac SS, Ata A, et al. Spontaneous pneumomediastinum: an extensive workup is not required. J Am Coll Surg 2014;219:713-7. [Crossref] [PubMed]
- Takada K, Matsumoto S, Hiramatsu T, et al. Spontaneous pneumomediastinum: an algorithm for diagnosis and management. Ther Adv Respir Dis 2009;3:301-7. [Crossref] [PubMed]
- Caceres M, Ali SZ, Braud R, et al. Spontaneous pneumomediastinum: a comparative study and review of the literature. Ann Thorac Surg 2008;86:962-6. [Crossref] [PubMed]
Cite this article as: Willems E, Pannecoeck K, Herpels V, Lerut P. Spontaneous pneumomediastinum: a rare cause of dyspnea. Curr Chall Thorac Surg 2019;1:4.