
Three-dimensional interactive quantitative surgical planning inferior pulmonary ligament approach VATS right S9+10 segmentectomy
Introduction
In recent years, video-assisted thoracoscopic surgery (VATS) has attracted much attention and has become a hot research field, because it has become a safe and effective surgical approach for stage IA non-small cell lung cancer (1). It’s difficult to expose and correctly identify the target vessels and bronchus, because them are commonly variable and deeply located in the lung parenchyma, beyond that, tailoring the intersegmental plane is also very difficult in VATS S9+10 segmentectomy (2-4). The three-dimensional reconstruction images can help us to understand the anatomic relationship of bronchi, pulmonary arteries and veins clearly, which is absolutely necessary for safe anatomy. A number of variations in the pulmonary arteries, veins and bronchi have been documented, and the preoperative recognition of the delineation is very useful in performing a safe segmentectomy. The three-dimensional reconstruction images have the advantage of a clear identification of the pulmonary vessel branches, even at the subsegmental and more peripheral levels. According to the anatomic variation of bronchus and vessels and the anatomic position of tumor, the 2 cm safe margin was measured, so as to define the scope of resection and make the operation plan, which can effectively solve the technical difficulties of pulmonary segmental resection, reduce the difficulty of operation and improve the treatment effect (5). This paper presented the three-dimensional interactive quantitative surgical planning inferior pulmonary ligament approach VATS right S9+10 segmentectomy (Video 1). All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s), and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this study and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Clinical summary
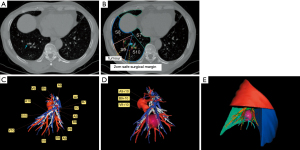
A part-solid ground-glass opacity (GGO) lesion had been identified at the right lower lobe in a 48-year-old female during incidental computed tomography (CT) screening 13 months prior to her presentation to us. Before admission, the patient underwent additional CT screening, and it indicated that the lesion had not significantly changed. CT imaging defined an 8-mm solitary part-solid GGO at the basal segments of the right lower lobe, with its density increasing over several months (Figure 1). The patient urged surgery. The radiologist diagnosed the GGO as minimally invasive adenocarcinoma. According to the National Comprehensive Cancer Network guidelines, the indication for sublobar resection is a peripheral nodule sized <2 cm with at least one of the following: pathological type is adenocarcinoma in situ (AIS), nodule with 50% GGO on CT, or radiological surveillance confirming a long doubling time (>400 days). Wedge resection was considered inappropriate for this case because of the location in the deep parenchyma, the lesion located too close to the intersegmental border, a combined segmentectomy would be performed. Family history was unremarkable, and she had never been a smoker. She was also assessed preoperatively to ensure that there was no evidence of metastatic disease.
Preoperative planning
Prior to the operation, the lesion location and the anatomy of the branches of the bronchus, arteries, and veins were defined using three-dimensional reconstruction images. The distance from the lesion to the intersegmental plane was measured in three-dimensional reconstruction images before the operation to ensure that the lesion was at least 2 cm away from the resection margin, the cut line is therefore determined. We proceeded with the inferior pulmonary ligament approach VATS right S9+10 segmentectomy (Figure 2).
Preparation before operation, anesthesia, positioning and port placement
Preoperative workup included clinical history, physical examination, lung function test, heart function test, blood gas analysis and basic examinations as usual. The positional relations of the basal segmental vessels and bronchi were preliminarily identified mainly through the three-dimensional reconstruction images. The patient was placed in the left lateral decubitus position. General anesthesia was induced, and intubation was achieved via a double-lumen endobronchial tube. The surgeon stands at the dorsal side of the patient, the assistant stands at the ventral side of the patient. The thoracoscope port was placed at the midaxillary line of the 8th intercostal space, about 1.5 cm long. The main utility incision was made in the 5th intercostal space at the anterior axillary line, about 3 cm long, while the assistant incision was located in the auscultation triangle, about 2 cm long. The incisions were protected with a silicone rubber wound protector.
Surgical techniques of right S9+10 segmentectomy
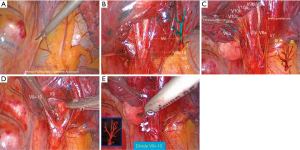
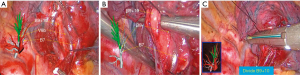
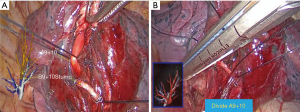
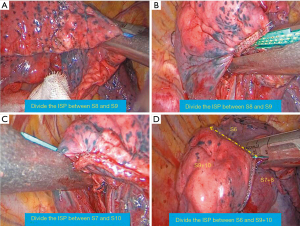
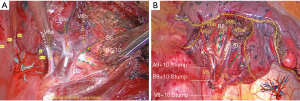
The basal segment of the lower lobe is relatively complex and variable, the S9+10 segmentectomy is a difficult operation. Three methods can be used: (I) interlobar fissure approach, this method was to start dissection from the interlobar fissure and make a tunnel between S6 and basal segments to expose the deep segmental hilum; (II) bidirectional technique, this method was initiated from the interlobar fissure and continued from “posterior approach”. The pulmonary artery is identified at the junction of the oblique and the transverse fissure. When the fissure is incomplete or inflammatory, this step can be tedious. Opening the fissure can lead to pulmonary tears and troublesome oozing, However, aside from concerns regarding possible torsion of S6 after complete separation, tunneling itself is itself a technically demanding procedure. The third method was the “Inferior lung ligament approach”, from the inferior view, the basal bronchus and its branches are located behind the veins, this method allowed segmentectomy of S9+10 performed without need to dissect the fissures and separate the S6 entirely. This report describes a case of tracking the target segmental branches by the three-dimensional reconstruction images during single-direction thoracoscopic S9+10 segmentectomy start from the inferior pulmonary ligament. First, the lower pulmonary ligament was dissociated, the inferior pulmonary vein is cleared from the surrounding tissues, and its basal branches are dissected (2,6). Confirm and transected V9+10 with intersegmental veins V8b and V6c preserved (Figure 1). After the vein branch is severed, we dissected of the lower lobe bronchus and resected the lymph node of station 13. The bronchial branches would be further dissected along the stems from proximal to distal (2). Confirm and transected B9+10 (Figure 3). After the bronchial branch is severed, the artery A9+10 can be seen. At the same level of the severed bronchus, the artery A9+10 was cut off (Figure 4). Regional lymph nodes were resected for intraoperative frozen section pathological examination (Figure 5). The method of inflation-deflation was used to identify the intersegmental plane. For the management of the intersegmental plane, we started from the relatively thin part of the lung tissue and gradually reached the segmental gate and the thick part of the lung. The specific steps were as follows: the first step is to open the boundary between S8 and S9, the second step is to open the boundary between S8 and S9 along the straight line where the lower lung ligament is located, the third step is to open the boundary between S7 and S10, and the last step is to open the boundary between S6 and S9+10 (Figure 6). The examination of frozen section confirmed minimally invasion adenocarcinoma. The view of the hilum after RS9+10 removal showed the stumps of targeted bronchi and vessels, the surgical margin width was greater than 20 mm (Figure 7). Finally, the lung was dilated, and air leakage was tested from the stump of the bronchus and the resection margin of the lung. A 10F thoracic catheter connected to the negative pressure drainage bottle was placed in the observation hole. The operative time was 2 h with an estimated blood loss of 50 mL.

Postoperative recovery
The patient recovered well and no occurrence of complications. The chest tube was removed on postoperative Day 3, the postoperative hospitalization time was 4 days, the final pathology revealed a pTmi1N0M0 minimally invasive adenocarcinoma. The chest X-ray on postoperative Day 3 revealed that the residual right lung expended well.
Comments
Pulmonary segmentectomy has been indicated for an increasing number of patients with early-stage primary lung cancer and a part of a benign lesion or a metastatic lung tumor. Compared with lobectomy, pulmonary segmentectomy was associated with equivalent oncologic outcomes in stage IA (T1aN0M0) NSCLC, but it can preserve more functional lung tissue. The favorable surgical results of segmentectomy have so far been reported (5,7-10). Because of the complex anatomy and many variations of segmental bronchi and vessels, thoracoscopic pulmonary segmentectomy is very delicate in technology. Especially, the anatomy of basal segment is more complicated. The bronchovesicular pattern of the right basal segments (S7, S8, S9, and S10) was the most complex, the branching patterns of segmental bronchus are B8 and B9+10 in the frequency of 86%, B8+9 and B10 in 8%, and B8, B9, and B10 in 6%. When S* is present (4% in frequency), care should be taken to differentiate between A10 and A*, and between B10a and B*. While the pulmonary artery usually branches into the A8 and A9+10 (90%) in frequency, it sometimes branches into A8+9 and A10 (8%), and A8, A9, and A10 in 2%. The branching patterns of right basal vein are V8+9 and V9+10 in the frequency of 30%, V8+9+10 and V10 in 14%, V8 and V8+9+10 in 2%, V8+9 and V10 in 26%, V8 and V9+10 in 18%, and V8, V9, and V10 in 10% (11). Hence one can see that, pulmonary segmentectomy of S9, S10, or S9+10 is probably the most challenging one among different types of segmentectomies, the pulmonary vessels and branches of the basal bronchi are located in the deep of the lung parenchyma, which is difficult to expose and trace accurately (2,4,12,13). In inferior pulmonary ligament approach, dissection proceeds from the pulmonary ligament to the hilum using the intersegmental septum as a landmark. We first encountered the inferior pulmonary vein, which has the most variations and combinations. This is key in identifying each branch of the inferior pulmonary vein. From this point of view, the lack of a reference and insufficient surgical experience and anatomical knowledge may lead to miscalculation in identifying the vein branches. The accurate establishment of the target vein is challenging and should be overcome in RS9+10 resection through the inferior lung ligament approach. Here we suggest that three-dimensional reconstruction should be introduced into the operation, given that it is a good tool to confirm the target segment vein and the intersegmental vein. Similarly, three-dimensional reconstruction can help in tracking the target bronchi and reducing unnecessary exploration. We do not need to expose all the branches of the artery because it does not affect the accurate identification of the target artery. The artery generally corresponds to the bronchus one by one and slightly deviates from the spine. Of course, we still need to confirm which approach will be more re-assuring through three-dimensional reconstruction.
In the process of operation, it is very important to understand the anatomical structure of patients by three-dimensional imaging and confirm it by many ways (14,15). The advantages of preoperative three-dimensional reconstruction are obvious, mainly reflected in the following aspects. First, the three-dimensional reconstruction can fully understand the spatial relationship and variation of each anatomical structure of lung segment before operation, and can display the three-dimensional direction of blood vessels. Second, three-dimensional reconstruction can accurately display the lung segment or subsegment where the nodule is located, and understand the relationship between the nodule and the blood vessels and trachea in the segment, which is conducive to determining the location during the operation. Especially for deep and untouchable nodules, the location of nodules is determined by locating the target segment. After determining the pulmonary segment where the nodule is located, the lesion can be resected by anatomical resection of the target segment. Third, the distance from the lesion to the intersegmental plane was measured in three dimensions before the operation to ensure that the lesion was at least 2 cm away from the resection margin,the cut line is therefore determined. For intersegmental veins, preserve them as far as possible under the premise of ensuring sufficient distance between the incision margins, otherwise sacrificial intersegmental veins should be chosen to ensure the incision margins. The segments for resection are determined based on tumor size and peripheral location in order to critically secure a segmental margin free of tumor cells. Fourth, the volume of the target segment and the proportion of the target segment in the lung lobe can be measured by three-dimensional reconstruction software before surgery. Fifth, we can make the operation programme and plan the operation steps.
Based on the three-dimensional interactive quantitative surgical planning, thoracoscopic segmentectomy for S9+10 can be performed successfully through the inferior pulmonary ligament approach. It also reduces the difficulty of operation and can be applied in most medical centers.
Acknowledgments
The video was awarded first prize in the First International Lung Surgery Competition (2019 Masters of Lung Surgery).
Funding: This work was supported by the Medical and Health Research Program (No. A20-2-015), Science & Technology Bureau of Yichang.
Footnote
Peer Review File: Available at https://ccts.amegroups.com/article/view/10.21037/ccts-20-74/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://ccts.amegroups.com/article/view/10.21037/ccts-20-74/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s), and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this study and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wisnivesky JP, Henschke CI, Swanson S, et al. Limited resection for the treatment of patients with stage IA lung cancer. Ann Surg 2010;251:550-4. [Crossref] [PubMed]
- Pu Q, Liu C, Guo C, et al. Stem-Branch: a novel method for tracking the anatomy during thoracoscopic S9-10 segmentectomy. Ann Thorac Surg 2019;108:e333-5. [Crossref] [PubMed]
- Kikkawa T, Kanzaki M, Isaka T, et al. Complete thoracoscopic S9 or S10 segmentectomy through a pulmonary ligament approach. J Thorac Cardiovasc Surg 2015;149:937-9. [Crossref] [PubMed]
- Endoh M, Oizumi H, Kato H, et al. Posterior approach to thoracoscopic pulmonary segmentectomy of the dorsal basal segment: a single-institute retrospective review. J Thorac Cardiovasc Surg 2017;154:1432-9. [Crossref] [PubMed]
- Wu WB, Xu XF, Wen W, et al. Three-dimensional computed tomography bronchography and angiography in the preoperative evaluation of thoracoscopic segmentectomy and subsegmentectomy. J Thorac Dis 2016;8:S710-5. [Crossref] [PubMed]
- Zhu Y, Pu Q, Liu L. Trans-inferior pulmonary-ligament VATS basal segmentectomy: application of single-direction strategy in segmentectomy of left S9+10. J Thorac Dis 2018;10:6266-8. [Crossref] [PubMed]
- Chujo M, Anami K. Branching patterns of segmental bronchi and arteries in the medial basal segment. J Bronchology Interv Pulmonol 2014;21:192-8. [Crossref] [PubMed]
- Okada M, Koike T, Higashiyama M, et al. Radical sublobar resection for small-sized non-small cell lung cancer: a multicenter study. J Thorac Cardiovasc Surg 2006;132:769-75. [Crossref] [PubMed]
- Shapiro M, Weiser TS, Wisnivesky JP, et al. Thoracoscopic segmentectomy compares favorably with thoracoscopic lobectomy for patients with small stage I lung cancer. J Thorac Cardiovasc Surg 2009;137:1388-93. [Crossref] [PubMed]
- Zhong C, Fang W, Mao T, et al. Comparison of thoracoscopic segmentectomy and thoracoscopic lobectomy for small-sized stage IA lung cancer. Ann Thorac Surg 2012;94:362-7. [Crossref] [PubMed]
- Nomori H, Okada M. llustrated Anatomical Segmentectomy for Lung Cancer. Heidelberg: Springer, 2012.
- Igai H, Kamiyoshihara M, Kawatani N, et al. Thoracoscopic lateral and posterior basal (S9 + 10) segmentectomy using intersegmental tunnelling. Eur J Cardiothorac Surg 2017;51:790-1. [PubMed]
- Sato M, Murayama T, Nakajima J. Thoracoscopic stapler-based "bidirectional" segmentectomy for posterior basal segment (S10) and its variants. J Thorac Dis 2018;10:1179-86. [Crossref] [PubMed]
- Shimizu K, Nakazawa S, Nagashima T, et al. 3D-CT anatomy for VATS segmentectomy. J Vis Surg 2017;3:88. [Crossref] [PubMed]
- Hagiwara M, Shimada Y, Kato Y, et al. High-quality 3-dimensional image simulation for pulmonary lobectomy and segmentectomy: results of preoperative assessment of pulmonary vessels and short-term surgical outcomes in consecutive patients undergoing video-assisted thoracic surgery. Eur J Cardiothorac Surg 2014;46:120-6. [Crossref] [PubMed]
Cite this article as: Liu Y, Zhang S, Che Z. Three-dimensional interactive quantitative surgical planning inferior pulmonary ligament approach VATS right S9+10 segmentectomy. Curr Chall Thorac Surg 2021;3:40.


