
Early stage of primary tracheal schwannoma mimicking a foreign body
Introduction
Schwannoma and neurofibroma are the main benign neurogenic tumors arising from the peripheral nerves. Schwannoma is much less common than neurofibroma; it is extremely rare in the trachea, being more frequently reported in the lungs and bronchi (1). Since tracheal schwannoma is exceedingly slow-growing, patients are generally asymptomatic until trachea reaches a critical size, at which point, obstructive symptoms are seen. Treatment options includes surgery and endoscopic resection.
Herein, we reported a clinical case of early stage primary tracheal schwannoma that was misdiagnosed as foreign body in a patient with asthmatic symptoms.
Case presentation
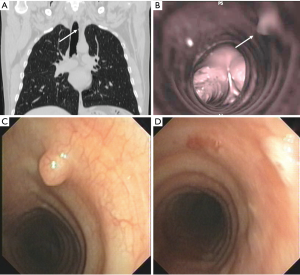
A 49-year-old no-smoker man with no other pulmonary diseases was referred to our hospital for management of asthmatic symptoms. He was treated with bronchodilators for several months without success. His past medical history was unremarkable except for accidental inhalation of a concrete fragment, occurred 9 months before the present admission. Physical examination, pulmonary function studies, and chest X-ray were negative. High Resolution Computed Tomography (HRCT) scan of the chest (Figure 1A) and virtual bronchoscopy (Figure 1B) showed a 2 mm hypodense lesion, located on the left lateral wall of the distal third of trachea; the tracheal lumen was within normal, and no other lesions were found into the mediastinum and/or the lung parenchyma. Under moderate sedation, patient underwent fiber bronchoscopy that showed the presence of a 2 mm round mass, in the distal third of the trachea. The mass was covered by normal tracheal mucosa with several small vessels on the surface, but was not pulsatile or friable (Figure 1C). In the same setting, the lesion was completely removed with standard biopsy forceps (Figure 1D). The entire procedure is summarized in Figure 2. Based on patient’s past medical history and endoscopic findings, the tumor was misdiagnosed as a foreign body.

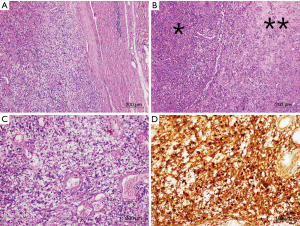
Histological evaluation showed an encapsulated spindle cell tumor (Figure 3A) with areas of high (Antoni type A) and low cellularity (Antoni type B) (Figure 3B), and vacuolated cell (Figure 3C). No signs of atypia were seen. The tumor was strongly and diffusely positivity for S-100 protein (Figure 3D) and vimentin, but was negative for cytokeratin, desmin, cluster of differentiation 117 and smooth muscle actin. The pathological results were consistent with a diagnosis of benign schwannoma. After resection of lesion, the symptoms completely disappeared, and no recurrence was found at two-year follow up.
Discussion
Primary tracheal schwannoma is an extremely rare clinical entity that accounts for less than 0.5% of primary tracheal tumors. Intrapulmonary neurogenic tumor was firstly described in 1914 (3); in 1951, Straus et al. reported the first case of schwannoma within trachea; from 1951 to 2013, 51 cases of primary tracheal schwannoma have been published in English literature (1,4,5). In all of these cases, the tumor occupied over 50% of the tracheal lumen; patients presented some non-specific symptoms like shortness of breath and dry cough, or repeated inspiratory dyspnea in serious cases. As most of the patients were initially misdiagnosed with asthma, the diagnosis was obtained by chest scan and/or bronchoscopy after an average of 17 months from the onset of symptoms. Treatments ranged from surgery to endoscopic resection using several devices as laser, electrocautery snaring, argon plasma, cryotherapy, and microdebridement (4-7). The choice was influenced by the characteristics of the tumor (pedunculated, sessile, presence of extratracheal component etc.…), and the risk of tracheal resection related to patient’s clinical condition.
The present case was unique as the tracheal schwannoma was incidentally diagnosed in a very early stage of disease. The HRCT scan of the chest showed a 2 mm hypodense lesion that was confirmed to be a solid endotracheal lesion by virtual bronchoscopic. Based on patient’s past medical history (he referred accidental inhalation of a concrete fragment several months before), lesion size (2 mm) and endoscopic findings (lesion covered by normal tracheal mucosa, not pulsatile or friable), the tumor was misdiagnosed as a foreign body. It was easily removed during flexible bronchoscopy using standard endoscopic biopsy forceps, without needing of complex endoscopic devices as previously reported (5-7). Surprisingly, pathological findings diagnosed the lesion to be a primary tracheal schwannoma. As the schwannoma originated from Schwann cells of sympathetic nerve (8), it likely stimulated the hyperactivity of bronchial mucosa with consequent asthmatic symptoms. This theory could explain the symptoms observed in our case, and their resolution after tumor resection.
Finally, our case under lights that primary tracheal schwannoma should be considered in the differential diagnosis of sudden respiratory distress or paroxysmal cough of unknown origin and resistant to bronchodilator treatment. The early diagnosis of tracheal schwannoma by HRCT and virtual bronchoscopy prevents the tumor growing and the needing of complex procedures for its treatment.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ccts.2019.08.06). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ge X, Han F, Guan W, et al. Optimal treatment for primary benign intratracheal schwannoma: A case report and review of the literature. Oncol Lett 2015;10:2273-6. [Crossref] [PubMed]
- The video edited the resection of the tracheal schwannoma. Asvide 2019;6:259. Available online: http://www.asvide.com/watch/32944
- Roviaro G, Montorsi M, Varoli F, et al. Primary pulmonary tumours of neurogenic origin. Thorax 1983;38:942-5. [Crossref] [PubMed]
- Hamouri S, Novotny NM. Primary tracheal schwannoma a review of a rare entity: current understanding of management and follow up. J Cardiothorac Surg 2017;12:105. [Crossref] [PubMed]
- Han DP, Xiang J, Ye ZQ, et al. Primary tracheal schwannoma treated by surgical resection: a case report. J Thorac Dis 2017;9:E249-52. [Crossref] [PubMed]
- Grillo HC, Mathisen DJ. Primary tracheal tumors: treatment and results. Ann Thorac Surg 1990;49:69-77. [Crossref] [PubMed]
- Melendez J, Cornwell L, Green L, et al. Treatment of large subglottic tracheal schwannoma with microdebrider bronchoscopy. J Thorac Cardiovasc Surg 2012;144:510-2. [Crossref] [PubMed]
- Shoji F, Maruyama R, Okamoto T, et al. Malignant scwannoma of the upper mediastinum originating from the vagus nerve. World J Surg Oncol 2005;3:65. [Crossref] [PubMed]
Cite this article as: Fiorelli A, Carlucci A, Cascone R, Panarese I, Accardo M, Franco R, Santini M. Early stage of primary tracheal schwannoma mimicking a foreign body. Curr Chall Thorac Surg 2019;1:13.


