
Surgical treatment for an infected traumatic pulmonary pseudocyst
Introduction
Trauma can cause many patterns of thoracic injuries including rib fracture, hemopneumothorax, constitution, pseudocyst, major vessel injuries or diaphragmatic injuries.
Among them, traumatic pulmonary pseudocyst (TPPs) is relatively rare, and decreases in size and resolves completely without specific treatments such as surgery in most cases (1). Therefore, the outcome of TPP is considered favorable when the patient has no other accompanied traumatic injuries.
Ulutas and colleagues reported that only 1 of 52 patients with TPP, which was enlarged up to 15 cm progressively, required surgical treatment (1).
Cho and colleagues also reported that there were no TPPs among 81 cases receiving additional invasive treatments after closed thoracostomy because none of them did not have any complications such as massive hemoptysis or infected TPP (2). However, surgical treatments can be required if the patient with TPP suffers from such complications because these complications can be life-threatening.
Here we report a successful surgical result of infected TPP, and review relevant literatures.
Case presentation
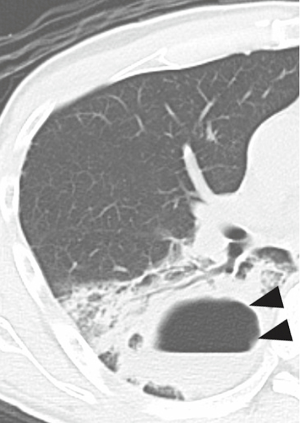
A healthy 41-year-old male patient was transferred to our hospital by a medical helicopter due to traumatic head and chest injuries. An initial computed tomography (CT) on admission revealed acute subdural hematoma and pulmonary congestion. Mechanical ventilation was introduced to keep respiratory status, however, he suffered from pneumonia as a result. Therefore, antibiotics were administered to treat the pneumonia. On hospital day 9, follow-up CT revealed emergence of infected pulmonary pseudocyst localized in right lower lobe (Figure 1). Although antibiotics administration was continued, the patient did not recover from the infection. Therefore, surgical resection of infected TPP was planned to control the infection.
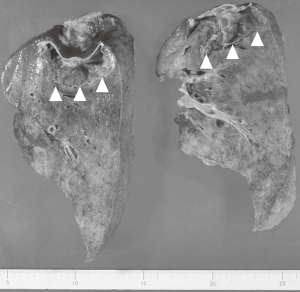
Under general anesthesia, posterolateral thoracotomy was performed on decubitus position. We did not choose thoracoscopic approach because lung swelling due to congestion was expected to prevent us from getting good surgical viewing. At first, we examined whether posterior segmentectomy of right lower lobe could be adopted or not in order to preserve pulmonary function. However, it was considered difficult because the pseudocyst was too large and we were not able to insert staplers in order to incise intersegmental plane because of lung swelling due to severe pulmonary congestion. Therefore, conventional right lower lobectomy was performed. The resected pulmonary pseudocyst contained frank pus containing multidrug-resistance bacteria in the cavity (Figure 2). Bronchial stump was wrapped by a flap of intercostal muscle.
The patient gradually recovered after removal of chest drainage tube on postoperative day 2, and was finally transferred to other hospital for the sake of rehabilitation.
Discussion
Thoracic surgeons or physicians sometimes treat TPP clinically although TPP is relatively rare disease among chest trauma. It is considered that TPP results from laceration or tearing of lung parenchyma, and air can enter through the laceration and create a cavity when a laceration causes only minor vascular damage and does not communicate with the pleural space. Subsequently, the air becomes trapped and the resulting cyst has no epithelial lining. As a result, connective tissue forms the lesion’s wall. Although most previous reports described TPP is caused by severe blunt trauma as well as our case, Ulutas et al. insisted that penetrating trauma also can cause TPP because the result in their article revealed there was no significant difference between the proportion of blunt trauma patients who developed TPP and the proportion of penetrating trauma patients who developed TPP (1).
TPP usually regresses spontaneously with conservative treatment (1,2). However, TPP may be treated if the patient has some complications such as hemothorax, pneumothorax, massive hemoptysis, or infection (3,4). Several authors reported infected TPPs which received additional surgical treatments, however, most of the literatures were written several decades ago (4,5). We speculate that recent advancement of antibiotic therapy can avoid progression of infection in most patients with TPPs. However, infected TPP sometimes becomes fatal when treated by only antibiotics administration. Carroll et al. reported that 4 patients with infected TPPs remained septic for weeks despite appropriate antibiotic therapy (4). While one of the four patients finally died of the infectious process, one patient successfully recovered after surgical treatment. The remaining 2 patients recovered from infection with antibiotics treatment alone, however, the course was prolonged. Our patient also did not recover from infection in spite of appropriate antibiotics administration. Therefore, we decided to perform surgical resection of TPP and finally got a successful result, suggesting the necessity of additional invasive treatments including surgery for infected TPP.
Gincherman and colleagues reported the successful results of CT-guided catheter drainage for a TPP instead of surgical resection of TPP (6). We performed surgical resection under general anesthesia because it was considered more radical. However, other less invasive treatments might be appropriate when the general condition is unstable due to injuries of other parts caused by trauma. Additionally, there are no reports describing appropriate surgical procedures to our best knowledge. In most previous reports, thoracotomy approach was chosen because these articles were written several decades ago (4,5). In our case, lung swelling caused by severe pulmonary congestion was expected to prevent us from getting good surgical viewing, and thoracoscopic approach gives surgeons limited surgical viewing. Therefore, we did not choose thoracoscopic approach
Conclusions
We experienced a successful surgical result of infected TPP. Although TPP is relatively rare disease among chest trauma and usually regresses spontaneously with conservative treatment, TPP may be treated if the patient has some complications such as hemothorax, pneumothorax, massive hemoptysis, or infection. Therefore, we should keep the necessity of surgical treatment in mind when we encounter the patients with TPP.
Acknowledgments
The authors appreciate all of the surgeons and coworkers who contributed to this study, and we thank the editors and reviewers for their assistance with the manuscript.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ccts.2019.08.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Informed consent is waived in our institution when the article is “Case Report”.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ulutas H, Celik MR, Ozgel M, et al. Pulmonary pseudocyst secondary to blunt or penetrating chest trauma: clinical course and diagnostic issues. Eur J Trauma Emerg Surg 2015;41:181-8. [Crossref] [PubMed]
- Cho HJ, Jeon YB, Ma DS, et al. Traumatic pulmonary pseudocysts after blunt chest trauma: Prevalence, mechanisms of injury, and computed tomography findings. J Trauma Acute Care Surg 2015;79:425-30. [Crossref] [PubMed]
- Gulbahar G, Gundogdu AG, Kaplan T, et al. Traumatic pulmonary pseudocyst due to thoracic trauma. Asian Cardiovasc Thorac Ann 2016;24:95-7. [Crossref] [PubMed]
- Carroll K, Cheeseman SH, Fink MP, et al. Secondary infection of post-traumatic pulmonary cavitary lesions in adolescents and young adults: role of computed tomography and operative debridement and drainage. J Trauma 1989;29:109-12. [Crossref] [PubMed]
- Ganske JG, Dennis DL, Vanderveer JB Jr. Traumatic lung cyst: case report and literature review. J Trauma 1981;21:493-6. [PubMed]
- Gincherman Y, Luketich JD, Kaiser LR. Successful nonoperative management of secondarily infected pulmonary pseudocyst: case report. J Trauma 1995;38:960-3. [Crossref] [PubMed]
Cite this article as: Igai H, Yoshikawa R, Ohsawa F, Yazawa T, Matsuura N, Kamiyoshihara M. Surgical treatment for an infected traumatic pulmonary pseudocyst. Curr Chall Thorac Surg 2019;1:10.


