
Complete superior vena cava resection for invasive thymoma
Introduction
Thymoma is the most common primary mediastinal tumour (1). It has the potential to invade mediastinal structures requiring complex surgical resection to gain clearance (2). Multimodality treatment with surgery, radiotherapy, and chemotherapy is currently adopted in the treatment of advanced thymoma. Complete en bloc resection of the thymus and involved structures with vascular reconstruction when required is the optimum surgical strategy.
Patient selection and workup
We present the surgical technique for resection of a thymoma invading the superior vena cava (SVC). Our patient was a 58-year-old male with an incidental finding of an anterior mediastinal mass. He had no symptoms suggestive of SVC obstruction.
Pre-operative preparation
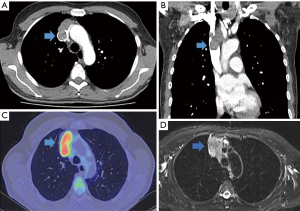
Computerized tomography (CT) scan showed a 55 mm × 41 mm mass invading the SVC. Positron emission tomography (PET) scan showed the mediastinal mass to be moderately avid with a standardized uptake value (SUV) maximum of 10.4 (Figure 1). CT-guided biopsy confirmed the mass to be a B2 thymoma. The patient consented to complete thymectomy and resection of the SVC performed via a sternotomy.
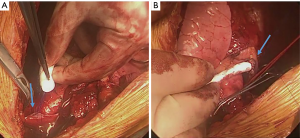
Procedure (Figure 2)

Median sternotomy was performed, and both pleurae were opened widely. No evidence of pleural involvement was seen. The mediastinal mass was seen invading the SVC and almost completely occluding it. The tumour invasion extended superiorly to partially invade the left and right brachiocephalic veins. Additionally, it was infiltrating the right upper lobe and pericardium. Although the right hemidiaphragm was not paralysed pre-operatively at the time of surgery there was tumour invading into the right phrenic nerve, and so this was resected.
We dissected out the left brachiocephalic vein and constructed a venous graft with a 10 mm × 14 mm GORE-TEX vascular graft using 4.0 Prolene having first given 5,000 units of heparin (Figure 3). We opened the pericardium and the graft was anastomosed to the right atrium. Correct sizing of the graft is essential to prevent kinking. This was followed by en bloc resection of the thymus and SVC with parts of the left and right brachiocephalic veins, along with a wedge resection of the right upper lobe, pericardium, and right phrenic nerve. The SVC was completely resected 3 cm above the junction to the right atrium using a vascular stapler. Distally, the right brachiocephalic vein was stapled 2 cm proximal to the junction of the right subclavian vein and internal jugular vein, and the left brachiocephalic was cut and oversewn at the midline. There was no hemodynamic instability during the procedure and inotropes were not required. Right hemi-diaphragm plication was also performed through the sternotomy using silk sutures. In our experience, a graft from the left brachiocephalic vein to the right atrium is sufficient for the venous drainage of the head and upper extremities. Although the patient can initially have issues with post-operative swelling, this quickly resolves.
Post-operative management
The post-operative course was uneventful, and the patient was discharged home on the eleventh post-operative day. Warfarin was prescribed for three months for the vascular graft. Histology showed a B2 thymoma with a clear resection margin and Masaoka-Koga stage three and T3N0M0. At the four-week follow-up clinic, the patient had recovered well and had no significant swelling of the upper limbs or face. His chest radiograph was satisfactory with normal position of the right hemi diaphragm. He has now finished his post-operative radiotherapy.
Tips, tricks, and pitfalls
SVC resection has been described previously for lung cancers and thymoma (4,5). Previous initial studies have reported clamping the SVC and then resecting and reconstructing it. In a study of 28 patients with non-small cell lung cancer, median clamp times were 40 minutes. Clamping the SVC can cause hypotension and cerebral venous hypertension, and the post-operative mortality rate from this series was 14% (5,6). More recent studies describe temporary SVC bypass during resection and reconstruction. A series of six patients undergoing SVC resection and replacement for lung cancer and thymomas reported performing a temporary catheter bypass prior to SVC resection and reconstruction. This was done safely without any post-operative mortality (5). Our technique of performing a graft from the left innominate vein to the right atrium, and then performing SVC resection prevented any hemodynamic instability and was sufficient for venous return from the head and neck. It avoided the additional steps of performing a temporary SVC bypass. For our technique to work, the patency of both brachiocephalic veins is required. If only one vein is patent then our technique can still be performed provided a side biting clamp can be placed on the patent brachiocephalic vein without significantly compromising venous blood flow.
Conclusions
Invasive thymoma is challenging disease, and a multidisciplinary approach is mandatory to achieve the best patient outcomes. Complete resection of the SVC, especially if completely invaded, is safe if alternative venous return can be constructed first. This approach avoids the need for SVC clamping or a temporary shunt. Surgery is challenging and should be performed by expert hands in high volume cardiothoracic centres.
Acknowledgements
Funding: None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Engels EA. Epidemiology of thymoma and associated malignancies. J Thorac Oncol 2010;5:S260-5. [Crossref] [PubMed]
- Girard N, Ruffini E, Marx A, et al. Thymic epithelial tumours: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2015;26 Suppl 5:v40-55. [Crossref] [PubMed]
- Asadi N, Barr J, Perikleous P, et al. Surgical technique: complete superior vena cava resection for invasive thymoma. Asvide 2019;6:129. Available online: http://www.asvide.com/article/view/31592
- Dai W, Dong J, Zhang H, et al. Superior vena cava replacement combined with venovenous shunt for lung cancer and thymoma: a case series. J Thorac Dis 2018;10:363-70. [Crossref] [PubMed]
- Spaggiari L, Thomas P, Magdeleinat P, et al. Superior vena cava resection with prosthetic replacement for non-small cell lung cancer: long-term results of a multicentric study. Eur J Cardiothorac Surg 2002;21:1080-6. [Crossref] [PubMed]
- Matsumoto K, Yamasaki N, Tsuchiya T, et al. Temporary bypass for superior vena cava reconstruction with Anthron bypass tubeTM. J Thorac Dis 2017;9:E614-E618. [Crossref] [PubMed]
Cite this article as: Asadi N, Barr J, Perikleous P, Anikin V. Complete superior vena cava resection for invasive thymoma. Curr Chall Thorac Surg 2019;1:2.


